Resources
Organizations & Reports
We’ve gathered trusted organizations, reports, and tools that support healthier outcomes for mothers and babies across North Carolina.
2018-2020 North Carolina Maternal Mortality Review Committee Report
This report reviews all maternal deaths in NC among state residents during 2018 through 2020, classifying them as pregnancy‐related or pregnancy‐associated. It identifies leading causes (such as mental health conditions, cardiovascular disease, infections, and substance use), timing of deaths (during pregnancy, within 42 days postpartum, or up to one year), and the proportion of deaths judged preventable. It offers actionable recommendations aimed at reducing maternal mortality, improving access to care, addressing mental health and substance use, enhancing emergency management, and strengthening system and provider responses.
2022-2026 Perinatal Health Strategic Plan
The NC Perinatal Health Strategic Plan serves as a statewide guide to improve maternal and infant health and the health of all people of reproductive age. The Plan includes three primary goals: addressing economic and social inequities; strengthening families and communities; and improving health care for all people of childbearing age.
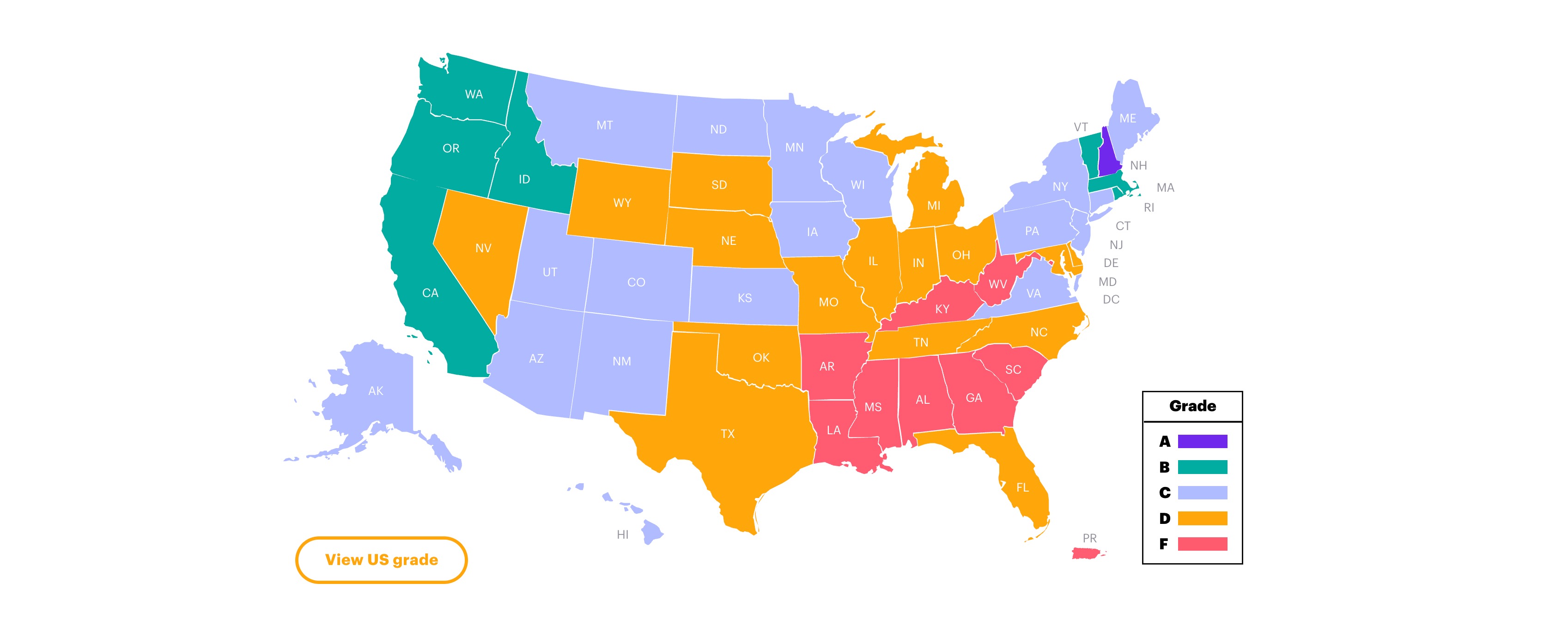
2025 State Report Card on Maternal Mental Health
A nationwide report that evaluates each state’s performance on maternal mental health care, including provider availability, screening practices, insurance coverage, and state initiatives. The report assigns grades by state (e.g., North Carolina) and highlights gaps in care, policy priorities, and areas for improvement.
5 Key Facts About Medicaid and Pregnancy
This issue-brief explains how Medicaid plays a major role in maternal care in the U.S., covering about 41% of births nationally and roughly half in many rural states. It outlines state‐by‐state eligibility trends, the impact of Medicaid expansion on access to care before and during pregnancy, extensions of postpartum coverage to 12 months, and how Medicaid supports maternity services beyond just delivery (e.g. mental health, home visits, doula support). It highlights disparities in eligibility and coverage cliffs that affect birthing people, especially in states without Medicaid expansion.
A Blueprint for Change: Safer Childbirth Starts in the Community
This article describes the Safer Childbirth Cities initiative, launched by Merck for Mothers, which partners with community-based organizations in U.S. cities bearing a high burden of maternal health disparities. It focuses on improving outcomes by engaging grassroots groups, redesigning care delivery in communities, addressing social determinants, enhancing patient voice and respect in care, and leveraging data to inform policies. The article outlines best practices and lessons learned from early adopters.
American College of Nurse-Midwives
ACNM sets the standard for excellence in midwifery education and practice in the United States and strengthens the capacity of midwives in developing countries. Our members are primary care, sexual, and reproductive providers for people throughout their lifespans, with a special emphasis on pregnancy, childbirth, and gynecologic and reproductive health.
Birth Doulas
What the Bump CLT is a professional doula service dedicated to providing comprehensive support throughout pregnancy, childbirth, and the postpartum period. Our team consists of Certified Birth Doulas who are credentialed through Novant Health and serve clients across Charlotte, North Carolina, and the surrounding areas.
Collaborative for Maternal and Infant Health
Collaborative that aims to improve the health and well-being of women and families across North Carolina through community partnerships, research and clinical care innovations, and developing new approaches to complex problems. Special focus on women with high-risk pregnancies and families with medically fragile infants.
DONA International
DONA International’s primary function is to provide excellent doula education and certification to a diverse population of doulas world-wide. DONA International promotes the highest quality perinatal support for pregnant, birthing, and postpartum people and their families by setting the standard for doula education and training, and by advocating the research-based benefits of doula care.
Doulas, once a luxury, are increasingly covered by Medicaid — even in GOP states
This article explores how many U.S. states—including several with Republican leadership—are expanding Medicaid to cover doula care. It discusses the benefits of doula services: lower rates of cesarean sections, reduced risk of preterm birth, increased postpartum checkups, and improved outcomes overall. The piece highlights policy changes in states like South Carolina, Montana, Utah, and Louisiana, examines challenges such as low reimbursement rates, and considers how funding uncertainty may affect access.
Every Baby Guilford
A collective action movement building collaborative solutions within Guilford County to disrupt longstanding health outcomes and racial disparities in infant mortality.
Family Forward NC
Family Forward NC® is an innovative initiative to improve the health and well-being of children and their parents and keep North Carolina’s businesses and workplaces competitive. It is employer-led change to increase access to research-based, family-friendly practices—big and small—that improve workplace productivity, recruitment and retention; grow a strong economy; and support children’s healthy development.
Healthy North Carolina and North Carolina State Health Improvement Plan
Healthy North Carolina 2030 is a set of health indicators with 10-year targets designed to guide state efforts to improve health and well-being. The State Health Improvement Plan operationalizes the priorities identified in Healthy North Carolina 2030.
Income insufficiency impacts early brain development in infants facing increased psychosocial adversity: A network-based approach
This study demonstrates that infants developing in a household where mothers reported income to be inadequate to support the family’s needs exhibit delays in brain maturation in the first year of life. This paper demonstrates the key role of adversity on the earliest stages of postnatal brain development.
Lactation Consultant Training Program
The LCTP is a comprehensive, accredited training program administered through the College of Business and Professional Studies Health and Human Performance Department at Johnson C. Smith University. The program provides supervised breastfeeding support education in the context of clinical lactation services and public health practice. Students receive didactic and clinical training and earn a minimum of 300 clinical hours and 90 didactic hours required for program completion and to comply with the requirements of an IBLCE-Approved Pathway 2 Program. Content considers equity, population and program-based applications, the social determinants of health, and factors and barriers specifically affecting people of color.
Leveraging an Academic-Practice Partnership to Improve Maternal and Child Health Outcomes in North Carolina
This article reports on the Improving Community Outcomes for Maternal and Child Health (ICO4MCH) initiative, launched by NC’s Division of Public Health in 2016 with funding by state legislation. It describes how local health departments partnered with UNC using a collective impact framework, implementation science, and a health equity lens to address three goals: improving birth outcomes, reducing infant mortality, and improving child health from birth to age five. Key strategies included shared metrics, implementation coaching, technical assistance, and community action teams. The article highlights barriers (e.g. staff turnover, balancing community needs with data demands, partnership sustainability) and lessons learned about scaling evidence-based maternal & child health interventions in local public health settings.
Listening to Women: Connecting Moms and Babies to Resources
Listening to Women is a free virtual home visitation and resource-connector program for individuals who deliver at MUSC Shawn Jenkins Children’s Hospital. It aims to identify and address barriers to postpartum success, support infant developmental milestones, and promote overall family health. The program includes a virtual nurse visit 5-7 days after discharge, text messaging for up to 12 months post-delivery to monitor social, physical, and mental health needs, and coordination with community resources via SC Thrive.
March of Dimes
March of Dimes is a national nonprofit that supports families before, during, and after pregnancy through research, advocacy, public health data tools, and community-based programs. In North Carolina, it offers the Ready for Life NC initiative (preconception health), detailed state “report cards” with maternal & infant health indicators (preterm birth, infant mortality, access to care), maternity care desert mapping, NICU family support, and material & digital education for expecting and new parents. These resources help identify health disparities, inform policy, promote access in underserved areas, and provide practical support for families and health professionals.
Maternal Outreach Through Telehealth for Rural Sites (MOTHeRS)
MOTHeRS is a multidisciplinary telehealth-backed outreach project launched in 2020 (with funding from the United Health Foundation) to reduce barriers to care for expectant and new mothers in rural eastern NC. It integrates maternal-fetal medicine, obstetrics, psychiatry, nutrition, diabetes education, and behavioral health into rural clinics and health departments to bring specialized care closer to home. The program also screens for food insecurity, links patients with community resources, and aims to reduce travel burdens, improve outcomes, and shrink geographic and health disparities. Among its achievements: thousands of telehealth and in-clinic patient visits, screening tens of thousands for food insecurity, distributing emergency food bags, and large reductions in travel miles for high-risk patients.
Maternal and Child Health Center for Policy & Practice
The Center was launched in 2025 by Heartland Forward to reduce maternal and child health disparities in the central U.S. It provides technical assistance, shares best practices, and uses data to support policymakers, providers, and community organizations. Key goals include implementing policy and regulatory reform (e.g. increasing Medicaid services, reopening labor & delivery units, bolstering workforce including doulas and midwives), improving access to prenatal and postpartum services, especially in rural & underserved areas, and aligning efforts across states using the National Governors Association playbook adapted from successful models like Nurture NJ.
Maternal and Child Health Equity and Action Network
The Maternal & Child Health Equity Action Network (MCHEAN) is led by the Foundation for Health Leadership & Innovation (FHLI) in North Carolina. Its flagship report, Rising Together, offers a community-informed landscape analysis of maternal and child health in NC and proposes cross-sector strategies in workforce, policy, system design, and funding to close equity gaps. MCHEAN brought together over 50 participants (half with lived experience) who co-created actionable plans for lasting change.
Maternal and Infant Health Innovation Center (MIHIC)
MIHIC is intended to serve as an anchor for maternal and infant health care services, social services and wraparound supports, data analysis and first-in-class research on maternal health care, a training and education site for the perinatal workforce, a catalyst of new innovations to drive improved maternal and infant health outcomes, and serve as a central hub for New Jersey’s stakeholders which include mothers and trusted community actors dedicated to improving the health of New Jersey’s babies and mothers.
NC Community Health Center Association
NCCHCA represents and supports North Carolina’s Federally Qualified Health Centers (FQHCs) and Look-alike community health centers serving medically underserved communities across many counties. Its members offer integrated care — medical, dental, behavioral health, pharmacy, vision, enabling services — regardless of ability to pay, often via sliding-fee models. NCCHCA provides training, technical assistance, governance & operational support, helps coordinate value-based payment arrangements through networks like the Carolina Medical Home Network, and acts as an advocate to state & federal policymakers. It also helps people locate community health centers near them.
NC Maternal Mental Health MATTERS
NC Maternal Mental Health MATTERS (Making Access to Treatment, Evaluation, Resources, and Screening Better) is North Carolina’s Perinatal Psychiatry Access Program. The vision is for all perinatal patients in North Carolina to have access to timely and high-quality mental health care and substance use treatment services. It offers free real-time perinatal behavioral health consultation for providers caring pregnant and postpartum patients, training and technical assistance, and patient resources. NC MATTERS is a collaboration between UNC School of Medicine, Duke’s Department of Psychiatry & Behavioral Sciences, and the North Carolina Department of Health and Human Services
NCCARE360
Searchable directory for health and human services resources
National Black Doulas Association
The National Black Doulas Association (NBDA) is a leading organization dedicated to supporting Black and BIPOC birthing families and birth workers. Its mission is to reduce Black maternal mortality and morbidity by building a professional, accessible directory of Black and BIPOC doulas, providing evidence-based training, and empowering doulas through education, mentorship, and community.
North Carolina Affiliate of American College of Nurse-Midwives
NCACNM is committed to setting the standard for excellence in midwifery education and practice in North Carolina. Our members provide healthcare throughout the lifespan, with a special emphasis on pregnancy, childbirth, and gynecologic and reproductive health.
North Carolina Chapter of the National Association of Certified Professional Midwives
NC for CPMs is focused on the work of advocating for expanded access to midwifery care. NC ACPM is the state professional organization for CPMs that not only works in the advocacy arena, but also provides opportunities for continuing educations, team building, peer review, peer to peer collaboration, and more to support the North Carolina midwifery community.
North Carolina Child Fatality Task Force
The North Carolina Child Fatality Task Force (CFTF) is a legislative study commission that examines the causes of child death and makes recommendations to the Governor and General Assembly on how to prevent child death, prevent abuse and neglect, and support the safety and well-being of children. The CFTF is part of the broader NC Child Fatality Prevention System created by state statute in 1991.
North Carolina Doula Organization
The NC Doula Organization supports and strengthens doula care in North Carolina through leadership development, education, community building, and financial support for doulas, especially those working in marginalized communities. They maintain a directory of doulas, offer peer learning (events like “Doula Connect,” “Lunch & Learn”), and advocate using a social-justice framework to make pregnancy, birth, and postpartum care safer and more equitable.
North Carolina Midwifery Education, Regulation, and Association
NCMERA is a collaborative work group of four state midwifery organizations dedicated to the advancement of midwifery in North Carolina and includes the North Carolina Chapter of the National Association of Certified Professional Midwives, The North Carolina Midwives Alliance, The North Carolina Affiliate of the American College of Nurse-Midwives, The North Carolina Friends of Midwives
North Carolina Perinatal Association
The North Carolina Perinatal Association (NCPA) is a statewide coalition dedicated to improving maternal and infant health through leadership, advocacy, and interdisciplinary education. Established in 1985, NCPA provides continuing education for perinatal professionals, fosters collaboration across disciplines (nurses, midwives, social workers, physicians, doulas, etc.), and advocates for policy and systemic improvements to support healthier pregnancies and births across North Carolina.
North Carolina Report Card: The State of Maternal and Infant Health
This report card tracks multiple indicators of maternal & infant health in North Carolina such as preterm birth rate, infant mortality, maternal mental health, prenatal care adequacy, low-risk cesarean births, and social/community determinants (e.g. maternity care access, environmental risks). It also includes data disaggregated by race/ethnicity to reveal health disparities. Policy measures like Medicaid postpartum coverage, doula reimbursement, midwifery support, and postpartum mental health screening are assessed. It’s meant to inform state policy, help stakeholders identify gaps, and promote equity in outcomes.
Perinatal Health Equity Collective (PHEC)
PHEC is a coalition of 500+ public, nonprofit, private partners, and people with lived experience across North Carolina committed to reducing perinatal health inequities. It serves as the backbone for the NC Perinatal Health Strategic Plan (2022-2026) — a roadmap focused on addressing economic and social inequities, strengthening families and communities, and improving health care for all people of reproductive age. PHEC oversees work groups and action teams (including maternal & neonatal levels of care, equity in practice, policy, data & evaluation) that develop policy recommendations, monitor dozens of health indicators, center community voice, and drive systemic change.
Perinatal Quality Collaborative of North Carolina
The Perinatal Quality Collaborative of North Carolina (PQCNC) is a statewide network of hospitals, clinicians, and health systems focused on improving care for mothers and newborns. Through evidence-based initiatives (such as eliminating elective early deliveries, boosting breastfeeding support, reducing neonatal infections, and strengthening data-driven care), PQCNC drives continuous quality improvement across the state’s perinatal systems.
Prenatal-to-3 Policy Impact Center Research for Action and Outcomes
The Prenatal-to-3 Policy Impact Center comprehensively reviews rigorous research to determine the state policies most effective at improving outcomes for infants and toddlers. The team of researchers and nonpartisan policy experts work directly with state leaders to empower states with rigorous evidence to implement effective and equitable policies that ensure all children thrive from the start. Investments in the earliest years benefit not only the child, but also society as a whole—leading to a thriving economy, strong families, and a proficient workforce.
Progress Toward Vitality: A 10-Year Retrospective Analysis of Systems Focused Efforts to Improve Maternal Health in Georgia
The Georgia Health Initiative publishes data-driven reports and policy analysis focused on Medicaid trends, maternal health outcomes, and strategies to achieve equitable health across the state. Their “Insights on Medicaid in Georgia” series and retrospective reviews (such as Progress Towards Vitality) inform public health work and help shape evidence-based decision-making for communities and policymakers.
Project CARA
Founded in 2014, Project CARA has supported over 2,500 pregnant and parenting people with substance use disorders. CARA prioritizes comprehensive, integrated care. The clinic, housed at MAHEC Ob/Gyn, provides medical, substance use, and additional support services so that patients can smoothly access the resources they need under one roof.
Reshaping Postpartum Care In Medicaid To Improve Outcomes And Reduce Costs
This article argues that extending Medicaid postpartum coverage to 12 months (beyond the traditional 60 days) is a key policy lever for improving outcomes and reducing long-term costs. It reviews evidence from states that have adopted or are adopting extended coverage, describes associated benefits such as reduced hospital readmissions, better access to continuous care (including mental and behavioral health), and how stretched services during the postpartum period correlate with worse outcomes. The article also discusses challenges states face (such as funding, administrative barriers, and aligning provider incentives) and offers recommendations on how to reshape care delivery, payment structures, and support systems to make expanded postpartum care sustainable.
Reshaping postpartum care in Medicaid to improve outcomes and reduce costs
This article discusses how expanded and more flexible Medicaid policies around postpartum care (e.g. extending coverage to 12 months) are showing promise for improving health outcomes for birthing people while reducing long-term costs. It reviews state-level policy changes, identifies gaps in existing postpartum care systems, and suggests reforms such as integrating mental health services, addressing social determinants of health, improving care coordination, and leveraging value-based payment models to better support postpartum individuals.
Sistas Caring 4 Sistas
Sistas Caring 4 Sistas is a women of color led birth justice nonprofit that is dedicated to improving the experiences and outcomes for pregnant, birthing, and postpartum people in Western North Carolina. They provide high quality doula care for birthing people of color, train the next generation of doulas and birth workers of color, and advocate for policy and systems changes that are rooted in community-based solutions to advance reproductive and social justice in our region.
Spotlight on Maternal Health
This NCIOM blog-/newsletter piece highlights ongoing efforts in North Carolina to reduce inequities in maternal health. It features work by the Perinatal Health Equity Collective (PHEC) through Maternal Health Action Teams focused on topics such as risk-appropriate care, workforce solutions, doula integration, and interventions for people affected by perinatal incarceration. It emphasizes centering community voice, cross-sector collaboration, policy recommendations, and “right care in the right place” strategies.
The Center for Native Health
The Center for Native Health's Mission is to support balanced wellbeing of southeastern Native communities in Western North Carolina through the preservation and respectful application of Native knowledge to empower the people, Land, and culture.
The Economic Case for Investing in Maternal Health
This report calculates the economic cost of poor maternal and infant health outcomes and describes how improved maternal health outcomes directly improve state economies.
The Fourth Trimester: A Crucial Phase for Women’s Health
This article discusses the “fourth trimester” (the postpartum period, especially the first 12 weeks and up to one year after birth) as a critical time for maternal health. It highlights how many pregnancy-related deaths and complications occur after delivery, including physical, emotional, and social health challenges. It emphasizes the importance of comprehensive postpartum care: early follow-ups, ongoing support for mental health, attention to social determinants (e.g. food security, housing, access to health resources), and improved coordination across providers.
The State of Birth Equity: Catalyzing Place-Based Philanthropy Impact Analysis (2025)
This 2025 report documents progress over three years of the SOBE initiative, which works with funders, community-based organizations, and state partners to advance birth equity through philanthropic alignment. It highlights successes in nine states, shares what’s been learned about seed funding, convening, policy alignment, and cross-sector collaboration. It includes lessons from state models (e.g. New Jersey) and emphasizes the value of trusting community power, flexible funding, and strategic partnerships to address systemic inequities in maternal and infant health.
Thriving Hearts Maternal Outcomes Initiative
Thriving Hearts is a multi-level intervention through local health departments to improve maternal health, with an emphasis on addressing hypertensive disorders in pregnancy - a major contributor to maternal morbidity and mortality. Thriving Hearts supports work in 10 counties in central North Carolina through 2030, focuses on both patients and health care teams, and partners academic experts, community leaders, and people with lived experience. Thriving Hearts is funded through a Patient-Centered Outcomes Research Institute (PCORI) Award
Triangle Doulas of Color
Triangle Doulas of Color is a doula agency providing pregnancy support, birth doula services, postpartum doula services, childbirth classes, placenta encapsulation, breastfeeding classes, lactation support, and a mom's group to build community among mothers and families in the Raleigh, Durham, Chapel Hill and surrounding areas of North Carolina.
Data Resources
We’ve gathered data centers, dashboards, and reports that contain maternal, infant, and child data to make it easier for people to access the data.

Maternal and Infant Health Data Dashboard
This dashboard brings together statewide maternal and infant health indicators, offering an at-a-glance view of trends, disparities, and outcomes to inform policy and program decisions.

State Center for Health Statistics (SCHS)
SCHS provides N.C. vital records, epidemiological data, and county health profiles that help track population trends, monitor public health needs, and guide evidence-based planning.

North Carolina Child Data Center
A comprehensive hub for data on child well-being in North Carolina, including health, education, and economic indicators used by advocates, policymakers, and community partners.

Maternal Mortality Review Report
This report provides data and an overview of all maternal deaths in the state with a primary focus on the patterns and trends in pregnancy-associated deaths.
The March of Dimes Report Card
An annual snapshot of maternal and infant health metrics across states, highlighting preterm birth rates, access challenges, and disparities to guide action and accountability.
Maternity Resources
We are in the process of adding more resources here, so check back soon or join our email list.